Dr Kandace McGuire, MD of VCU Massey Cancer Center reveals how she’s changing the standard of breast surgery

Last week, Dr Kandace McGuire, MD of VCU Massey, Virginia, took part in a fascinating webinar on changing the standard of breast cancer care, in which she revealed how the Magseed® marker and Magtrace® lymphatic tracer are revolutionizing her surgery practices.
In the online session, hosted by our North American distribution partners Mammotome, the leading physician spoke about wire-free lesion localization and radiation-free sentinel lymph node biopsy (SLNB), as well as the advanced techniques of targeted axillary dissection (TAD) and ‘delayed’ sentinel lymph node biopsy (dSLNB) .
Dr McGuire’s views on improving lesion localization
To begin, Dr McGuire shared her frustrations towards the guidewire, describing the method as outdated and too inaccurate for modern times. Non-wire solutions were praised for the flexibility they offer, the ability to more precisely localize lesions and their enablement of advanced oncoplastic techniques.
“The problem is that these [wires] must be done the day of the procedure, impacting on scheduling between surgery and radiology”
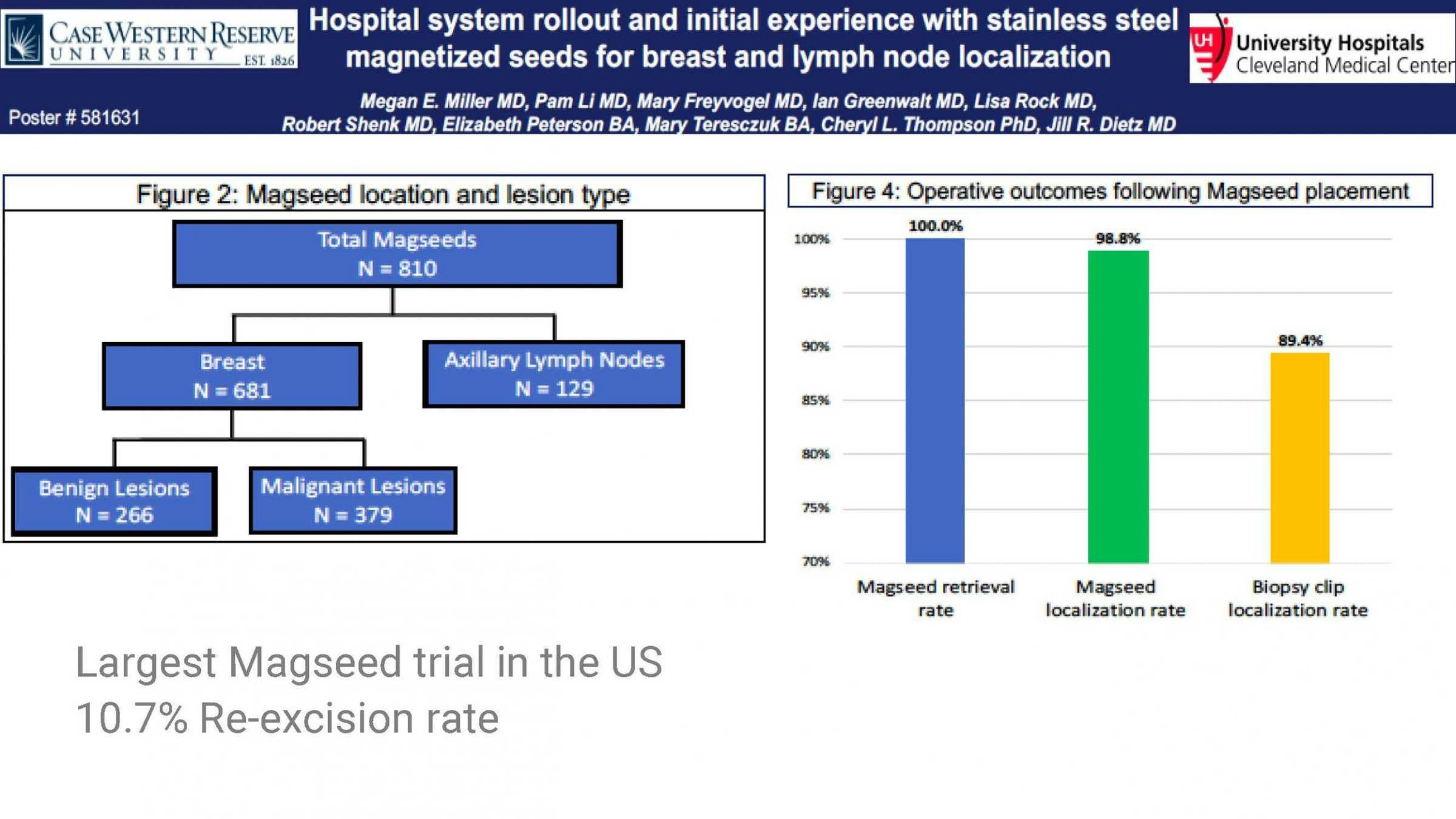
In support of choosing to use the Magseed® marker, Dr McGuire shared a key study from University Hospitals Cleveland Medical Center, presented at ASBrS 2019.
This study was both the largest Magseed® trial in the US and largest study of non-radioactive seeds in the world, with 810 markers placed for lesion and lymph node localization. All were successfully retrieved with a minimal re-excision rate of just 10.7%.
Outside of the Magseed® marker’s use for lesion localization, Dr McGuire then explained the practice of utilising it for the TAD procedure.
It was shown how clipping a node prior to chemotherapy with a Magseed® can significantly help reduce your false negative rate when applied alongside a SLNB.
Dr McGuire’s views on more effective axillary management
On the topic of SLNB, the dual tracer choice of combining Tc99 and blue dye was praised for its effectiveness for identifying sentinel lymph nodes, but its potential drawbacks were also highlighted.
Drawbacks mentioned included the potential risk of anaphylactic shock in some patients who receive blue dye and the short half-life of Tc99, which can restrict scheduling options - plus, the pain to patients that accompanies its application.
Dr McGuire explained how the tonicity of Magtrace® helps to combat concerns of patient pain and how its longer lasting properties opened up more flexible OR scheduling.
To finish the session, Dr McGuire discussed the relatively new phenomenon of delayed SLNB.
It was explained how the procedure - which has been shown in clinical trials to allow 78.3% of patients to avoid an SLNB (Karakatsanis, 2019) - involves injecting Magtrace® prior to surgery, then performing a lesion localization to analyze if the DCIS is invasive, before committing to lymph node surgery.
“This technique something I got very excited about the first time I heard about it, and I’ve done it a few times and it works really, really well”
This feedback echoes a number of surgeons who have begun incorporating dSLNB into their treatment pathways, with the Magtrace® lymphatic tracer the only known solution that can be used to perform this procedure.